Diabetic Retinopathy
Patients with diabetes run a greater risk of experiencing eye related compilations than patients who do not suffer from diabetes. The most common complications include cataract, glaucoma, retinopathy, retinal vein occlusion, anterior ischemic optic neuropathy, decrease of the corneal sensitivity, extracranial nerve palsy, neovascular glaucoma.
Diabetic Retinopathy
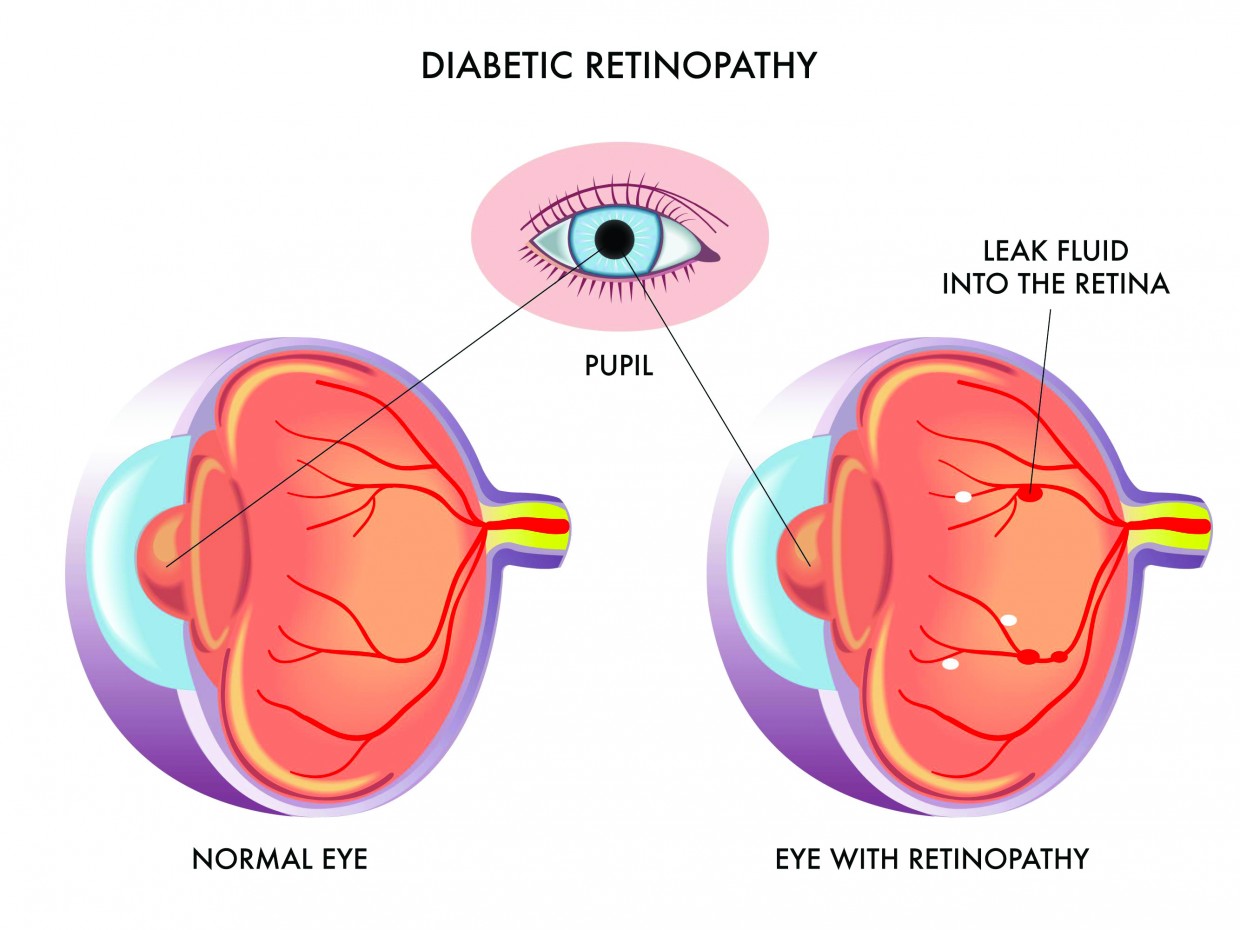
Diabetic Retinopathy is a chronic, progressive disease of the small vessels of the retina, that is related to increased blood sugar levels. The retina is the inner layer of the eye, where light rays are transformed in electric signals which are then transferred to the brain. Diabetic retinopathy is the most common cause of blindness in patients between 35-55 years of age in Europe.
Classification
The classification of diabetic retinopathy is based on the clinical examination.
The initial stage is non-proliferative diabetic retinopathy. This stage is characterized by damage of the wall of small blood vessels which lose their tightness and become leaky. In uncontrolled diabetes, retinopathy progresses to the next stage which is the proliferative type.
This stage is characterized by the occlusion of the vessels and the formation of new vessels which develop either in the optic disc or in other areas of the retina. New vessels do not have the characteristics of healthy blood vessels and they may therefore bleed causing vitreous hemorrhage.
New vessels may also evolve in fibrous tissue, which develops on the surface of the retina, causing tractional retinal detachment.
The development and worsening of diabetic retinopathy is related to:
- Type of Diabetic Control
- Arterial hypertension
- Hyperlipidemia
- Duration of diabetes
- Genetic predisposition
Diabetic retinopathy may cause vision loss in one of the following ways:
- Formation of new vessels which may cause vitreous hemorrhage and/or tractional retinal detachment, and
- Macular edema or ischemia which causes loss of the central vision.
Macular edema
The macula is the most sensitive part of the retina and controls the central vision of the eye. In diabetes, alterations in the capillary walls cause the leakage of various fluids, resulting in accumulation of fluid in the macula.
This fluid build-up in the macula is called diabetic macular edema and can cause loss of vision. The macular edema may accompany both types of retinopathy: proliferative and non-proliferative. Macular edema may be focal or diffuse, ischemic or of mixed pathology.
Treatment of Diabetic macular edema
When the macular edema has caused significant visual loss, the following are administered:
- Intraocular injections of Anti–Vascular Endothelial Growth Factor Drugs (anti-vegF) and/or
- Laser in the macular area
Diabetic proliferative retinopat
- Panretinal photocoagulation is administered to patients with proliferative retinopathy.
- Vitrectomy is recommended to patients with vitreous hemorrhage and/or tractional retinal detachment.
Panretinal photocoagulation
It is carried out in 2-3 sessions, during which approximately 1000 burns are delivered to the retina. The aim of the treatment is regression of new vessels that characterize proliferate retinopathy.
Technique
At first, mydriasis is performed, i.e. mydriatic eye drops are instilled to the eye to dilate the pupil. Mydriasis usually requires 20-30 minutes. The pupil may stay dilated for 4-6 hours. Mydriasis causes blurring of the vision, especially during reading. Mydriasis is required for most fundus conditions since it is required for fundoscopy, Optical Coherence Tomography, photograph taking, fluorescein angiography, administration of intravitreal injections or retinal photocoagulation (laser), etc.
Prevention
Diabetic proliferative retinopathy is less common than non-proliferate retinopathy and is related to an increased risk of permanent vision reduction.
Patients with diabetic retinopathy may remain asymptomatic until the final stage. This practically means that even an eye with normal vision (10/10) can suffer from proliferative diabetic retinopathy.
Therefore, an annual fundoscopy is recommended from the time of diagnosis and for life. It is also recommended that the patient regulates their blood sugar as well as other conditions such as high blood pressure and hyperlipidaemia for the prevention/treatment of retinopathy and macular edema.
